Mother Jones Illustration; Getty
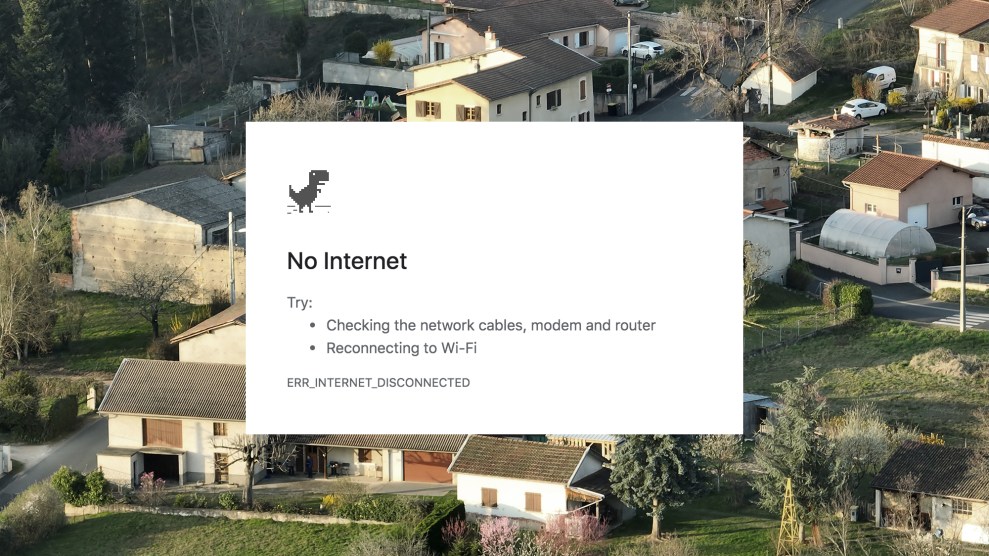
On New Year’s Eve 2021, the federal government launched the Affordable Connectivity Program, which has helped over 20 million American households afford internet access with monthly subsidies of $30 (or up to $75 on some tribal lands). But funding for the program is set to run out in April unless Congress acts by Friday—depriving many of those homes of vital resources, especially access to online telehealth.
People in rural communities are more likely to have issues accessing the internet than those in suburban and urban areas, with nearly 25 percent saying internet access is a major issue. But rural areas also face profound shortages of local doctors, which has increased the importance of telehealth, and the CDC has repeatedly found in the past decade that telehealth is an effective tool in helping rural patients manage chronic health conditions such as home-based rehab after strokes and diabetes.
While telehealth services existed before Covid, and were used to reach patients in rural areas, pandemic stay-at-home orders increased access to virtual appointments, and more doctors now use internet-based telehealth to see some patients. Experts who spoke with me agreed that cuts to internet access could worsen existing healthcare disparities.
Katy Schmid, a senior director at The Arc, an organization serving people with intellectual and developmental disabilities, leads an initiative to help people with these conditions maintain steady internet access. She’s concerned about the impact that ending the Affordable Connectivity Program would have on disabled patients. “This end of funding will most certainly impact folks with disabilities who access telehealth, specifically folks in rural areas who are unable to drive,” Schmid said.
“While not all healthcare services can or should be delivered remotely, telehealth has increasingly become an indispensable component across various healthcare settings,” Kathy Hsu Wibberly, director of the University of Virginia’s Mid-Atlantic Telehealth Resource Center, told me. “When certain populations are excluded from accessing telehealth services, it inherently becomes a health equity issue.”
Telehealth appointments for some people far from healthcare clinics or specialists can be the only timely way to see a doctor, says Dr. Kevin M. Curtis, medical director of Dartmouth Health Connected Care and Center for Telehealth. Drawing on his experience working in northern New England, Curtis notes that academic medical centers tend to have more specialists “with profound specialty shortages elsewhere.”
Even fully funded, the Affordable Connectivity Program hasn’t closed all broadband gaps when it comes to telehealth. Nearly a fifth of Dartmouth Health outpatient telemedicine visits for its patients in Vermont, a largely rural state, are audio-only due to technology barriers, including broadband ones—which, Curtis says, “is not fair to them.”
Unstable internet access has other health care impacts, according to Dr. Lisa Adams, who oversees Dartmouth College’s Center for Global Health Equity. “We tell patients all the time that the [patient] portal is the most secure means for sharing health information,” Adams said, “but you need to have reasonable internet access to use it.” Adams, while finding telehealth very useful, also hopes to see more funding for healthcare providers to be able to do home visits in more rural areas.
Continuing to expand access to the internet would build telehealth equity, which “fundamentally is about providing equal opportunities for individuals to receive care via telehealth,” Hsu Wibberly said, “irrespective of their social, economic, or geographic circumstances.”