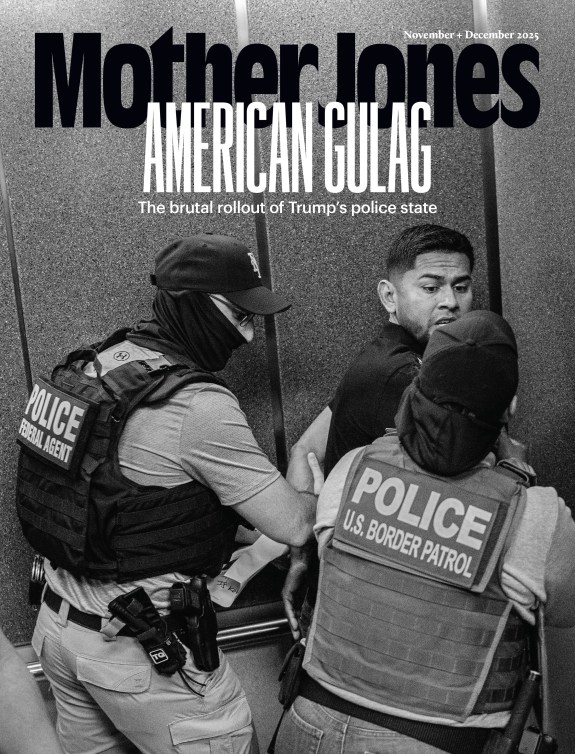
Myung J. Chun / Los Angeles Time / Getty
On March 5, Californians will vote on Proposition 1. The ballot measure, if passed, will allow the state to divert funds raised for non-coercive mental health care to housing and other behavioral health programs—including involuntary confinement.
Through a bond, the proposition would also raise some $6.4 billion (over 30 years) for behavioral health and housing. But almost as much—a further $140 million annually—would be taken directly from the state’s mental health budget, redirecting it from community mental health services to behavioral programs such as residential substance abuse treatment and centers for short-term involuntary psychiatric holds. Counties would also have to spend another third of their MHSA funds on housing and the costs of forced treatment.
Proposition 1 would enact and fund two bills that made their way through California’s legislature with bipartisan support. In amendments immediately before the final vote in September, legislators moved to strike language requiring any mental health facilities created with the funds to be voluntary and unlocked. After signing those bills, California Gov. Gavin Newsom said the legislation would “prioritize getting people off the streets, out of tents and into treatment.” A recent estimate pegs the state’s homeless population at more than 180,000, a 12 percent increase from the year before. A major factor driving homelessness in California is the state’s lack of affordable housing.
“For months,” said Clare Cortright, policy director of advocacy group CalVoices, Newsom insisted that all treatment facilities set up with Prop 1 funds would be “community-based, voluntary, [and] unlocked… until he was blue in the damned face.”
Exactly how much of the money will be redirected into institutionalization is up in the air, but more than $4 billion could potentially go into building locked behavioral health facilities and placing Californians in them. Fiscally, according to the Legislative Analyst’s Office, the 30-year bond would cost the state around $310 million annually, above and beyond the existing mental health funds it would divert.
Many disability advocates in California are wary that Proposition 1 falls into a pattern of increasing coercive institutionalization that targets those living with psychiatric disabilities and substance abuse disorders—such as expansion of CARE (Community Assistance, Recovery, and Empowerment) courts, which compel people to follow a treatment plan overseen by a judge to avoid legal action or conservatorship. Critics, like Human Rights Watch, have expressed concern that the program coerces defendants into taking potentially harmful medication. A key component of the fight for disability rights in the United States has been opposition to institutionalization—around 5 percent of disabled people lived in institutions between 2012 and 2016— and criminalization of disabled people’s presence in public, such as historical Ugly Laws.
Nearly $2 billion of the bond could go to permanent supportive housing. Ryan Dougherty, professor of medical ethics at Baylor College of Medicine, doesn’t see that as inherently bad—more housing is needed “to better serve what is a very structurally vulnerable population.” But, Dougherty. adds, problems arise when “attaching housing to involuntary treatment programs.” That approach might lead to coercive treatment, rather than fulfilling a “basic human necessity.” Longer-term, more intensive treatment programs, according to some disability advocates, aren’t inherently bad either—in the absence of involuntary treatment and coercion.
At a California Assembly committee hearing in August, disability and housing advocates also questioned why funding for the state’s serious housing crisis would have to cut into mental health funds. In 2004, Californians approved the Mental Health Services Act, which raises $2 billion to $3 billion annually in tax revenue to help counties fund programs for community well-being. In the years that followed, according to the independent, public policy–focused Steinberg Institute, participation in MHSA-funded programs decreased homelessness and incarceration—and a 2021 analysis suggests that the act’s funding also helped reduce alcoholism-related deaths.
California is “setting the example for the rest of the country in terms of how to design and fund mental health programs,” Dougherty says, and should show more concern about expanding involuntary treatment. Some voters have also found the legislation unusually confusing: the text explaining the ballot measure, at 68 pages, is the longest in a California voter guide since at least 2010. Its more visible backers are the state’s Building and Constructions Trades Council and the prison guard’s association; opponents, in addition to CalVoices, include the state’s League of Women Voters and Disability Rights California.
Advocates of preserving MHSA funding point to its direct positive impact. The recipients can be wide-ranging: in addition to grants for more typical mental health providers, it also supports peer-driven projects like Oakland’s Black Men Speak, which encourages men of color to share their mental health experiences through storytelling.
Eric, a high schooler, was referred to the Community Youth Center of San Francisco after a family conflict. Through the center, which receives MHSA funds, he now attends a photography-based support group, attending events where he and others can practice photography, and others where the group discuss their work and check in with each other about life. Eric calls it “a great relief to have a support group behind me.”
Like other state initiatives, the MHSA is not without flaws: in 2023, an Orange County-focused case study found that there weren’t enough programs helping people who spoke languages like Farsi and Korean.
But its funding, says Marcia Miller, a San Francisco State University lecturer and mental health clinician, can help cover the costs of care, allowing patients without insurance to see providers and get support.
In comparison, Miller cautions, when someone is forced into institutionalization, “they come back out, they’re released, and they did not receive the services that they actually needed”—and, as a bonus, they may mistrust mental health services thereafter.
Data shows that the state has been steadily increasing funding for residential facilities that sometimes lock patients in for weeks at a time, and funding few community residential treatment centers, which are modeled after a home environment and less restrictive than psych wards. Gov. Newsom has called these latest grants “a key part of how California is transforming the approach to helping people.”
Cortright contends that the billions raised by Prop 1 would help pay for the rise in institutionalization that’s being fueled by California’s diversionary CARE courts.
“They’ve got a cost for that person being in a treatment facility, and they can use MHSA funds,” Cortright says. “That’s where the money goes.”