Go Nakamura/Getty
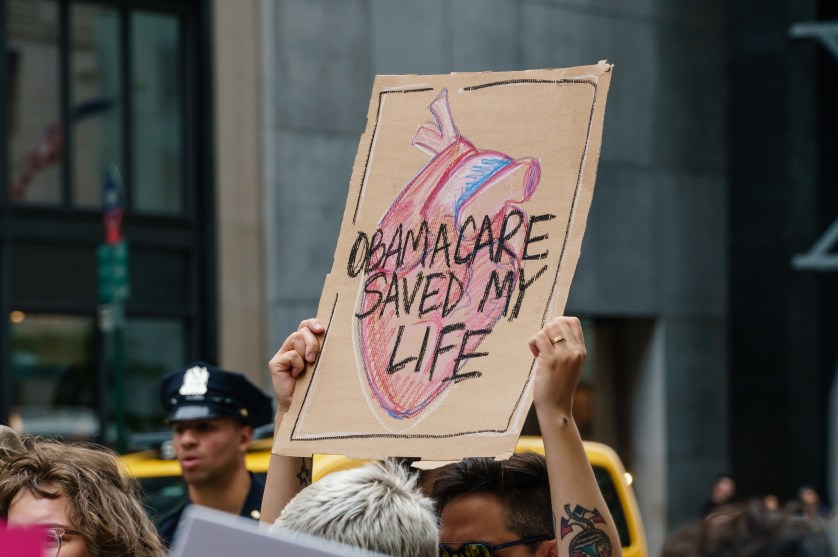
Starting tomorrow, states will begin to terminate health care coverage for people who no longer qualify for Medicaid, marking the end to a pandemic-era rule that automatically renewed coverage for Medicaid recipients even if they were no longer eligible. An estimated 15 million Americans, a majority of whom are low-income, are expected to lose their health insurance before the end of the year.
The emergency policy was created at the start of the pandemic under the Families First Coronavirus Response Act which prevented states from kicking off Medicaid recipients regardless of whether they had filled out the necessary paperwork to re-enroll. During the pandemic, the program saw 20.2 million new recipients over the course of two years, according to the Kaiser Family Foundation. With the end of the pandemic-era requirement, states will return to checking people’s Medicaid eligibility by requiring recipients to fill out forms to verify their personal information, income, and household size—a massive administrative effort for families likely economically struggling.
According to a Department of Health and Human Services analysis, the 15 million expected to lose coverage include an estimated 5 million children; Black and Latino households will be disproportionately affected. Others at risk of losing their insurance include: individuals who have moved out of state during the pandemic, people with limited English proficiency, and those with disabilities.
Arizona, Arkansas, Idaho, New Hampshire, and South Dakota will be the first states to end coverage. Most states will move to do the same in either May or June.