PeopleImages/Getty
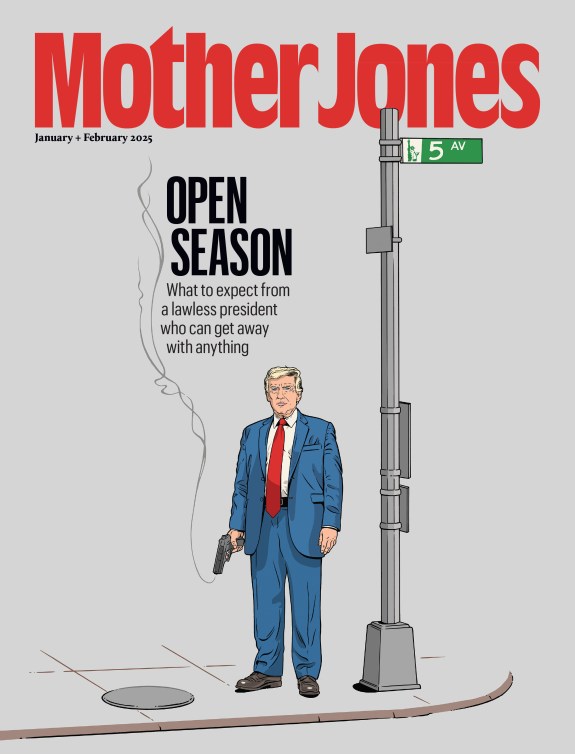
Editor’s note: After reading Mother Jones reporter Julia Lurie‘s work on the opioid crisis, a former journalist contacted us with his own story of addiction. The following is his narrative, in his own words. In order to protect his privacy, we have not included his name.
On a sunny September morning in 2012, my wife and I returned to our apartment from walking our eldest daughter to her first day of kindergarten. When we entered our home, in the Washington, DC, suburb of Greenbelt, Maryland, I immediately felt that something was off. My Xbox 360 and Playstation 3 were missing.
My wife ran to the bedroom, where drawers were open, clothing haphazardly strewn about. It was less than a minute before a wave of terror washed over me: My work backpack was gone. Inside that bag were notebooks and my ID for getting into work at NBC News Radio, where I was an editor. But the most important item in my life was in that bag: my prescription bottle of Oxycodone tablets.
“I can’t believe this happened to us,” my wife said.
“They took my pills,” I said.
We repeated those lines to each other over and over, my wife slowly growing annoyed with me. Why didn’t I feel the same sense of violation? Why wasn’t I more upset about the break-in? Oh, but I was. Because they took my pills. The game consoles, few dollars and cheap jewelry they stole would all be replaced. But my pills! They took my fucking pills!
We had to call the police. Not because of the break-in but, rather, so I could have a police report to show my doctor. That was all I could think about. My pills.
How did I become this person? How did I get to a place where the most important thing in my life was a round, white pill of opiate pleasure?
Before 2010, I only had taken opiates a few times. In 2007, I went to the emergency room in my hometown of Cleveland, Ohio, because I could not stop vomiting from abdominal pain. Upon my discharge, I was given 15 Percocets, 5 milligrams each. I took them as prescribed, noticed that they made me feel happy, and never gave them another thought.
After I took a reporter job in Orlando, I began to get sick more frequently, requiring several visits to the ER for abdominal pain and vomiting. In September of 2008 I was diagnosed with Crohn’s, an inflammatory bowel disease, and put on a powerful chemotherapy drug called Remicade to quell the symptoms. My primary care doctor, knowing I was in pain, prescribed me Percocet every month. I took them as needed, or whenever I needed a pick-me-up at work. I shared a few with a coworker from time to time. We’d take them, and 20 minutes later, start giggling at each other. I never totally ran out—never took them that often. I never needed an early refill.
In March of 2010, I was hired as the news director of a radio station in Madison, Wisconsin. Before we moved, my doctor in Orlando wrote me a Percocet script for 90 pills to bridge the gap until my new insurance kicked in in Wisconsin—approximately three month’s worth. I went through them in four weeks. I spent about a week feeling like I had the flu and then recovered, never once realizing that I was experiencing opiate withdrawal for the first time. Soon after, I set up my primary and GI care with my new insurance, and went back to my one-to-two-pills-per-day Percocet prescription, along with a continuation of my Remicade treatment.
Two months later, while my wife and daughter were visiting family in Cleveland, I developed concerning symptoms. My joints were swollen, I couldn’t bend my elbows, I was dizzy. I went to the ER, where for two days the doctors performed all sorts of tests as my symptoms worsened. Eventually, the rheumatologist diagnosed me with drug-induced Lupus from the Remicade. I was prescribed 60 Percocets upon leaving the hospital.
When I went back to my GI doc four weeks later for a refill, he told me he was uncomfortable prescribing pain medication, so he referred me to a pain clinic. I told the physician there how I would get cramps, sharp pains that would sometimes lead to vomiting. Did it hurt when I drove over bumps, or when bending over? Yes, sometimes. I left with a prescription for Oxycodone, with a prescription to take one pill every three to four hours. My initial script was for 120 pills. I felt like I hit the jackpot.
Soon those pills weren’t doing it for me. I told the doctor I needed to take more just to feel any effect. So he upped my script to 180 pills a month and added a new script for 60 extended-release morphine pills.
I often found myself barely functioning at work or at home, always nodding off into a doped-up stupor. My second daughter was born in November of 2010. There is a picture of me “sleeping” while sitting up on the couch, holding her in my arms. Looking at that picture now, it breaks my heart. I don’t remember much about this time in my life—just that it was cold and snowy and dreamlike and dark, and I didn’t much like Madison.
Sometimes I would ask my pain management doctor what my “exit” plan was for getting off these pills. I shouldn’t worry, he said—I needed the meds. I was in good hands, he assured me. He was monitoring my usage.
In April 2012, when I was hired by NBC News Radio, we moved to Washington, DC, where finding pain meds proved to be quite a challenge. The DC area was far ahead of the rest of the country when it came to opiates, and many doctors didn’t touch Oxycodone. I began to worry whether I had made a mistake by leaving my more permissive doctors in Madison.
I finally found a doctor who would see me, about 45 minutes outside of DC in suburban Virginia. He was a young doctor with a new urgent care practice. After marveling at how much pain medication I was on, he reluctantly prescribed me the Oxycodone and morphine, but said he would only cover me until my insurance kicked in. The feds were monitoring prescriptions and he didn’t want to lose his license.
The next challenge was filling my scripts. It was near impossible to find a CVS or Walgreens that kept Oxycodone pills in stock. Pharmacies didn’t want the hassle. The DEA was coming down on them. Though I lived in suburban Maryland, I would have to drive across the city into rural Virginia to find a CVS that carried the pills and was willing to fill my prescription. I went through this dance for two months.
Eventually my insurance kicked in and I could afford to see a real pain management doctor, who, like the urgent-care doc, could not believe how many opiates I took on a daily basis. The doctor told me that we were eventually going to have to “do something” about this. He asked for my complete medical records, hoping to understand why I was on such high doses. This guy would end up saving my life.
While all this was happening, my wife was starting to worry about me. My behavior had changed over the few years I took the heavy doses of opiates. She saw me nod off. She saw my mood sour and lighten, up and down. I carried pills with me wherever we went. I became obsessed with video games, which are a lot of fun when you’re high. I got sick a lot, but the pills didn’t seem to help. And there were more and more reports of people dying from their opiate prescriptions. She didn’t know how to address this topic with me. She tried once or twice and I became defensive. I needed my pills, I would say. Why would the doctors give them to me if they weren’t safe?
And then we had the break-in.
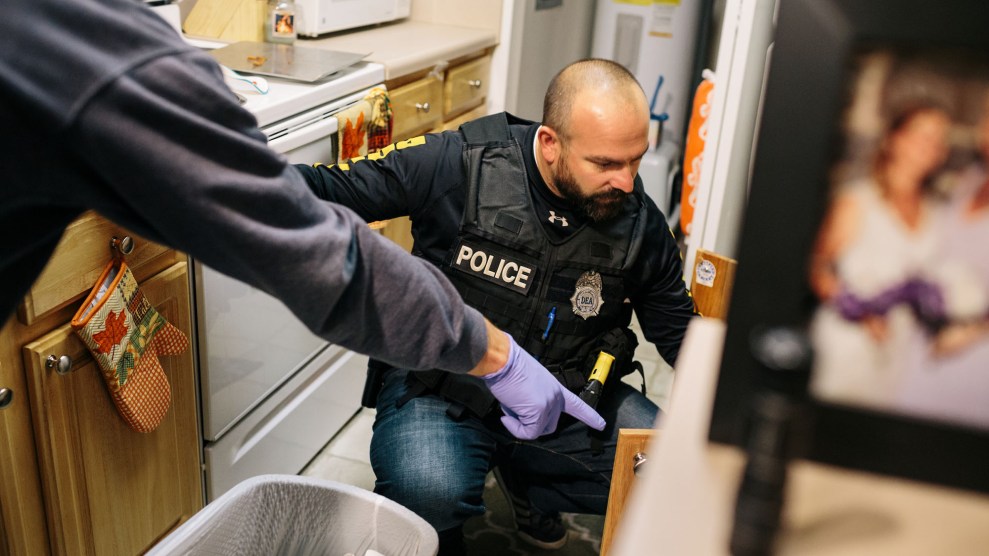
I didn’t get a report from the police that day. It takes several days, apparently. I didn’t know this, and I freaked out. The officer gave me a case number and his phone number and said the doctor was welcome to follow up for verification. A day later I drove to the pain clinic, which squeezed me in after I told them I couldn’t wait two weeks to see the doctor.
When the doctor came into the room I began telling him what happened and thrust the piece of paper with the case number and officer’s number at him. I’m sure I looked like a maniac. He smiled, set the piece of paper down on the table, and told me that it was time I got off the pills. A week prior, one of his patients died from an overdose. He was reevaluating everything. He told me that the pills were actually making me sicker, irritating my Crohn’s symptoms. With my increasing dose, I was becoming more sensitive to pain. That’s why I didn’t feel better. That’s what sent me to the ER over and over. In fact, he couldn’t believe that no one figured this out in Madison (or wanted to, he inferred). He was incredulous as to the high doses I was on. It was a miracle I was still alive. He said he was going to refer me to a doctor who would prescribe Suboxone, the brand name of a drug called buprenorphine that curbs cravings for opioids. It was time I got off the pills.
I didn’t panic. I didn’t freak out. I felt relief. I started to cry.
After seeing the Suboxone doctor for the first time, he told me to stop taking the pills right away. I would see him in 24 hours. I needed to be in withdrawal before I could take the Suboxone, as that’s the only way it works.
Those were a very exciting 24 hours. Though I went into withdrawal quickly, just knowing there was a solution on the other end got me through. I didn’t sleep well, couldn’t eat. I was on the toilet quite a bit. But I felt strong, empowered. I was getting off the poison forever.
The next day he evaluated me and deemed me ready. He wrote a script for one week of Suboxone, 14 strips. I would dissolve one strip under my tongue twice daily. I had to go fill the script at the pharmacy around the corner and come right back to his office. He would make sure the dosage was working and then send me home. In a week I would come back for an evaluation and we’d take it from there.
I called him about 45 minutes later in full panic mode. The withdrawal was still there, the medicine wasn’t working, I said. He told me to take another strip and to call back in an hour.
One hour later a relief washed over me like none before. I didn’t feel high—I felt normal. For the first time in several years I felt like me again. Color returned to my world. I could feel my life. My emotions were real, no longer numbed. I called the doctor while looking out over the backyard of my complex with tears streaming down my face, breathing in the night air.
“Thank you for this,” I said. “Thank you for helping me get my life back.”
Over the next five years, much of my life changed, most of it for the better. However, I’m still on Suboxone, taking it twice daily. It’s a lot more convenient than the alternative drug, methadone, which must be administered at a clinic.
For the past few years doctors have simply prescribed Suboxone to me—I think this is because I always appear quite “normal.” I’m a professional with a family. Maybe I don’t look like I’m addicted to drugs, but I didn’t press the issue and neither did they. No one ever asked about my addiction, or whether I had any unresolved issues.
Until now. A few weeks ago, my family and I to moved to Germany to live with my parents. At first, I was ecstatic: What a wonderful opportunity for my kids.
But then, reality struck. Suboxone. How would I obtain my Suboxone? Would I be able to get my Suboxone? What would happen if I couldn’t get my Suboxone?
As a former radio newsperson, I was used to moving and reestablishing my care in a new town. The dance was always the same: I provided my medical history, sang my sad story and showed my current prescription. Because I have a clean history without abuse, no early refills, and I was not an illegal user, I never had a problem finding a new provider.
I had an excellent relationship with my doctor in the Bay Area, and she was more than willing to write a letter that I could show my doctor in Germany, letting him know that I was a compliant patient with her program and I had clean urine screens. In the Suboxone world, that’s a ringing endorsement. It’s what any Suboxone provider wants to know about their new patient—is this guy going to waste my time?
As strict as we might think the American system is now when it comes to opiate replacement therapy, in regards to getting a script and managing care, it’s far more regulated in Germany. I learned that when I went to see my doctor for the first time this week.
He’s a very kind man, maybe just a few years older than I, and he understood my situation. As I’ve explained, I’m in this “one-percenter” category. I was not an opiate abuser. I am taking Suboxone as a result of overprescribing. However, as he explained to me, Germany doesn’t really care about that. All substitution-therapy patients are lumped into the same group, and I could end up in a nightmare scenario where I’m having to go to the pharmacy every day for up to six months to receive my Suboxone. It’s treated just like methadone here. That means no vacations, no overnight excursions to Italy or Austria with the family.
The other option is to make a case for me taking Suboxone for pain. It’s not a commonly used drug for that purpose, but if my doctor can show my history of Crohn’s, my journey through pain management, and how I wound up here, it would present a reasonable case that could be approved.
So I’m in the process of chasing down my records back to my diagnosis in 2008. I’m a bit nervous, because I only have a few more weeks’ worth of script left.
One day I hope to be off Suboxone forever. But with six months of language classes on the horizon, followed by several years of university study to be an interpreter in communications, I’m not sure when I’ll ever have the time for withdrawal and detox. How frustrating that, more than seven years later, the shadow of opiates looms over everything I do, no matter how far I run.