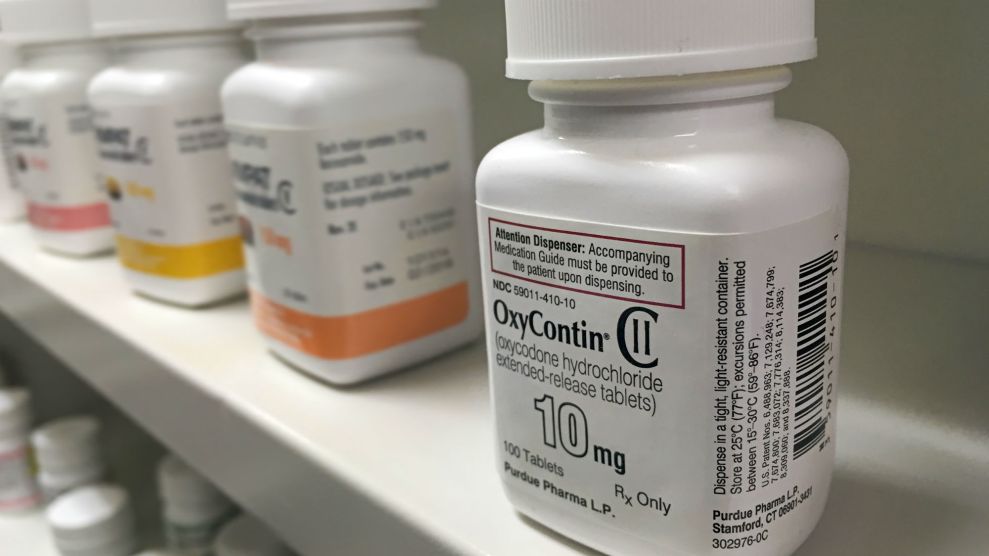
<a href="http://www.istockphoto.com/photo/oxycontin-bottle-on-shelf-gm578596836-99485787?st=_p_oxycontin">Pureradiancephoto</a>/iStock
Scientists are one step closer to designing a drug that relieves pain but doesn’t have the harmful side effects of today’s opioid painkillers.
The need is clear: In 2014, 14,000 Americans died from overdoses involving prescription opioids like oxycodone or hydrocodone (known by brand names OxyContin and Vicodin). The death toll from prescription opioid overdoses has roughly quadrupled since 1999. The drugs, prescribed for chronic pain, frequently lead to addiction; as many as one in four people prescribed opioids for long-term pain struggles with addiction, according to the Centers for Disease Control. When ingested in high doses, the drugs slow down breathing and can be fatal.
A team of researchers, whose work was published earlier this month in Nature, designed a compound named PZM21 that is producing promising results. Multiple experiments on mice appear to reduce pain without slowing down breathing or being addictive. When the rodents treated with the compound were placed on a hot plate, for example, they appeared to experience as much pain relief as those treated with morphine. Mice showed no preference between being in a chamber where they received PMZ21 and another where they received a saline solution.
Rather than tweaking an existing drug, as most drugs are created, the research team used a combination of computational modeling and synthetic drug generation to design a compound from scratch that would bind well with the known structure of the brain’s opioid receptors. Doing so was a four-year effort, involving researchers from Stanford University, the University of North Carolina at Chapel Hill, the University of California-San Francisco, and Friedrich-Alexander University in Germany.
Of course, there’s a long way between mice studies and a drug on the market for human use; the authors estimate it will be one to two years until the compound makes its way to the Food and Drug Administration for testing. Still, when it comes to developing a drug that could help mitigate today’s opioid crisis, Aashish Manglik, a Stanford physiologist and the study’s lead author, says he is “cautiously optimistic.”