Thinkstock/suemack
The latest book from surgeon and best-selling author Atul Gawande may not change your whole life, but it could very well improve how it ends.
In Being Mortal, Gawande, a longtime staff writer for the New Yorker, takes on the utter failure of the medical profession when it comes to helping people die well, and the short-sightedness of the elder facilities that infantilize people rather than bother to figure out what they actually need to maintain a modicum of meaning in what’s left of their lives. In the process, he gives us a lesson on the basic physiology of aging and on the social and technological changes that led to most of us dying in hospitals and institutions rather than at home with our loved ones. And he chronicles the rise of the nursing home and the creation of assisted living as its antidote—if only it were.
The picture can seem pretty bleak. Many of Gawande’s subjects are dealing with the always-hopeful oncologists who, rather than accept the inevitable, coax their patients into trying futile fourth-line chemotherapies that nobody can pronounce. And then you’ve got hospitals axing their geriatrics departments (aging Boomers be damned) because Medicare won’t cover the extra costs of making someone’s last years worth living. There’s also a deeply personal aspect to the book, which goes on sale today. Gawande recounts the recent travails of his family, which began when his father, also a surgeon, was diagnosed with a cancer that would slowly eat away at his physical capabilities and ultimately end his life.
But Being Mortal is hopeful, too, and that’s why it could make a difference. Most of the changes we need to make aren’t expensive. Indeed, some of them could save us a bundle in cash and needless suffering. It turns out, for example, that terminal patients in hospice programs often live longer and better than their counterparts in treatment. In fact, the mere act of talking with caregivers about what you value as you near the end of your life leads to a longer one. Gawande also introduces us to quirky visionaries who took it upon themselves to improve matters. My favorite was Bill Thomas, a young doctor who somehow convinced state regulators to let him turn a nursing home into a menagerie. “I mean, he was a crazy-man!” Gawande told me with a laugh when I called to grill him on the details. But sometimes that’s what it takes to wake people up.
Mother Jones: In the book, you write about how, hundreds of years ago, there used to be these very popular guidebooks instructing people on how to die well. Have we, as a society, forgotten how to do that?
Atul Gawande: Well, the definition of what it means to be dying has changed radically. We are able to extend people’s lives considerably, including sometimes, you know, good days. And we’ve also completely changed the family structure. People live alone for long periods of their elder years. So those guidebooks don’t fit our world. But we haven’t got another plan. The current plan is “Hmm, you’d better go to the ER.”
MJ: How can the medical profession be so oblivious to people’s needs?
AG: It’s because of this mismatch in our values. The profession has been focused on ensuring people’s health, so safety and survival are the assumed priorities, and we don’t know how to cope when they don’t actually add up to well-being for people. Well-being can be trying to just have a good day today. Or, being with my dogs matters hugely. Or, I’ve got a life project that’s really important. Or, I’m trying to get to a wedding on Saturday, and it means the world to me. Those are things we’ve had zero interest in, in the medical context.
MJ: You describe a University of Minnesota study that followed a large group of independent elderly people over 10 years. Half of them continued consulting with their primary care doctors as needed. That was the control group. The others, members of the test group, were assigned a geriatrics team. What happened?
AG: Those folks stayed independent for far longer. They were admitted to the hospital less. And the other key result is that the hospital didn’t have money to keep the geriatricians going, so they got rid of the department entirely. [Laughs.] So it was this incredibly successful result in serving needs that people have, but we also demonstrated that we don’t have any will or interest in sustaining it.
The geriatricians have training in basic skills that we’re not teaching other people—97 percent of medical students never learn about geriatric skills. What are some of those skills? They are things like understanding that, for people who reach certain levels of frailty, more important than getting their mammogram, more important than getting their blood pressure tweaked, they’re at high risk of falling. If they fall and break their hip, they not only die sooner, they die miserably.
Geriatricians know how to help keep people from falling: They know how to examine the feet so that you can recognize problems that can make you, as one patient put it, “tippy.” There are combinations of medications that can make patients dehydrated and dizzy and more likely to fall. There are nutritional signs and approaches that can make people more weak and unable to stay stable. And you can address those things. Meanwhile, you have people who are being trained like me. I know exactly what to do if we want to try to do a procedure. But if the aim is help them keep from falling and be independent in their home as long as possible, I didn’t know what to do.
MJ: A lot of doctors don’t seem to get that caring for the very old and treating them can be two entirely different things—which can be mutually exclusive. Or is it that they do get it, but for some reason don’t act accordingly?
AG: No, I think we don’t get it. One of the things that’s really striking about meeting geriatricians or palliative care physicians or hospice nurses is that they treat the observation of the patient and the conversation with the patient the same way I treat operations. They regard it as something requiring tremendous skill and practice to pay attention to the details. And that means even breaking down the words you use in a conversation so you’re able to understand what somebody else’s life is really like and what their priorities are. Or to have observations where you’re able to watch them terribly closely and see what is happening in their lives. It’s these basic detective skills and conversational skills that most people in medicine have simply not developed.
MJ: Given the demographic trends, the fact that hospitals are cutting geriatrics programs now just seems insane.
AG: It’s total insanity! And hospitals are doing it because we’re not valuing those capabilities in society. No one is clamoring for geriatricians. You know, if we took away the ability to put defibrillators in people in their last years, people would be shouting in the streets. But take away the capacity to see a geriatrician and there isn’t a murmur. Because it requires admitting that we have mortal lives. The second part of it is that these are the lowest paid people in the profession and the fact that we value those skills so poorly. It’s foolish: These are folks that keep people out of hospitals, out of emergency rooms, out of nursing homes. And not only that, they help people achieve more fulfilling lives. We’ve clearly got the priorities wrong.
MJ: There’s also hospice, which we see as this program you go into when you’re about to die. But it turns out that’s kind of ironic, right?
AG: Yeah. The evidence is that people who enter hospice don’t have shorter lives. In many cases they are longer. I kept a series of studies that really help bring it out. One looked at lung cancer patients who were at stage four and lived on average only 11 months. Half of them were randomized to usual oncology care, the other half randomized to oncology care plus early discussions with palliative care physicians who would discuss the patients’ aims and goals for the end of life. The group who had those conversations chose to stop their chemotherapy sooner. They had fewer days in the hospital. They were less likely to die in an ICU. They started hospice earlier, and they lived 25 percent longer. And that’s largely because, you know, that fourth round of chemotherapy or that last ditch operation is vastly more likely to be causing you harm than it is to be providing you benefits. So over and over again we end up sacrificing people’s lives and making them more miserable—which is just bad decision-making all around.
MJ: You’d think insurers would be clamoring for more geriatricians. I think the way you put it in the book is that, if these end-of-life discussions were an experimental drug, the FDA would immediately approve it.
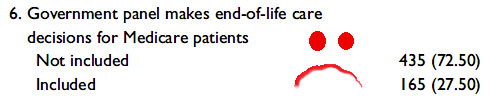
AG: Yeah. You know, we had this difficult time politically where the notion that these conversations are really important got polarized. Part of the reason I wrote this book is to try to pave a path beyond that polarized discussion. I think we can easily value having these conversations, but the question is, what kind of conversation? If the conversation people think is coming is the “death panel” conversation, like “Yeah, you can’t have the kind of care that you want,” that’s a total failure. If the conversation that we reward doctors to take the time for are conversations about, “What are your priorities in life, and how do we make sure that we’re not sacrificing them as we go along this course of care?” That’s what the evidence indicates will make a huge difference.
MJ: In the book, you point out that as of 1945 most people still died at home. By the 1980s, we were mostly dying in hospitals and nursing homes. How did we end up outsourcing our mortality?
AG: I think the story goes back a long way, and I see it happening it India, where my family is from. When we lived in a society where we had large families that lived together, especially in agricultural societies like my grandfather and father grew up in, the result is you always had family around to take care of you. My grandfather died at 110, still in the family home. He sat at the head of the table, and people brought decisions to him about the business and about the family, marriages, and he was tremendously respected even though he was still someone who needed help getting to the bathroom and putting his clothes on.
We’re nostalgic for that time, but the reason it worked is because young people were enslaved, especially young women. And the economic progress of society—ours in the 19th century, India/China/Korea in the present time—has come because we’ve allowed young people to follow their dreams: work where they want, live where they want, marry whom they want. They’ve moved to the cities, they’ve left the elderly behind, and we don’t have a plan. The plan that we therefore default to is, well, as long as they can live independently, things are fine, but if they start having trouble that’s a medical problem.
Medicine’s core value is to sacrifice your time now for the sake of possible time later. It has not been oriented toward saying, “What do we do to make it possible for someone to have their best possible day now, as they face the waning of their years or the limitations of their body?” We created nursing homes in that image. Heck, we call them nursing homes [laughs] out of an inability to admit that they exist for managing the process of being a mortal person. So that’s the place we ended up: We have medicalized aging. And that experiment is failing us.
MJ: On the positive side, you profile folks who’ve kind of figured things out, like Keren Wilson, one of the pioneers of assisted living, who set out to eliminate nursing homes. What’s the primary difference between her version of assisted living and a lot of what now passes for assisted living?
AG: I think the key difference is the recognition that you’re doing more than just keeping people safe. Part of the idea is that you might be able to get up and go to the kitchen and open the refrigerator and pick out something you want to eat. Well, for many people in nursing homes, we’ll say, “That’s not safe.” They might end up drinking a soda, and that’s not healthy if you’re diabetic. Or you might have an Alzheimer’s patient who goes to the refrigerator and instead of grabbing the pureed options, they grab a cookie and try to eat it. The pleasure of having some solid food, even if it’s risky, is a choice that people want to still be able to make.
Keren Wilson, at the age of 19 her mother had a stroke and was left permanently disabled; she went from one nursing home to another, and all she wanted was the freedom to wake up whenever she wanted, keep her collection of knick-knacks and tchotchkes, to have some privacy and be allowed to lock the door, to not always have a roommate—all these things that are pretty fundamental to having a life you feel is worth living. And that’s what Wilson created. But assisted living today has ended up most often being subsumed by this idea that safety comes first.
MJ: So you basically become a ward.
AG: Yeah. You become a member of the asylum.
MJ: You also profile this doctor, Bill Thomas, who takes a job in a nursing home, finds it horribly depressing, and then proceeds to try something as simple as it is radical. Give us the elevator version.
AG: He decided that what he wanted to do to combat what he called “the three plagues”—hopelessness, helplessness, and boredom—was to bring animals into the nursing home! He brought in dogs and cats and 100 parakeets. And would hand out a pair of parakeets that would actually be owned by the residents themselves to look after. Treating them as if they were capable of caring for something, not just passive wards of the caregivers, was dramatically transformative. People came out of their shells. They had a purpose. They ended up achieving lower amounts of medication use for things like anxiety and psychosis. They not only became more active and found life having more worth to it, they also lived longer.
MJ: That’s a great story.
AG: Part of what I’ve got to get across is what a crazyman he is! The nursing home director starts saying, “Well, the regulations say we can’t have any birds, because they’re absolutely unsafe. And we’re allowed one dog, and we have to get an animal handler.” And Thomas says, “Well, what if we got two dogs?” And “what if we got two cats—for every floor?” And “what if we bring 100 parakeets in?” You know, until everybody’s eyes are bugging out. [Laughs.] He was just sort of relentless.
MJ: Well, he got his way. So, this book was also deeply personal. Your family came face to face with a lot of these things after your father was diagnosed with cancer. Is this what prompted you to tackle the topic?
AG: Almost certainly. My father died from a cancer of his brainstem and spinal cord in 2012. He was diagnosed several years before that, and right around that time I started doing research for an essay that first appeared in the New Yorker and then it became the whole book. I don’t think I would have admitted at that time that what my father was going through was a major motivation—and yet it clearly became that. Because as I learned more about how to talk with my patients, I started applying the same ideas to how we would ensure that my father didn’t have this kind of anonymous, institutionalized end. That we would able to pave a different path for him.
MJ: Do you think this book might help pave a path that makes things different when you’re old and infirm?
AG: I certainly hope so. You know, the idea that just because you can’t walk anymore or you can’t eat the food you used to eat, that therefore you don’t have a contribution to make or you can’t be the leader of your own life? That is depressing. And I think the existence of places and people who are showing you how it’s possible to be otherwise is incredibly helpful. But it’s still only a minority of what’s available. It doesn’t cost more. It’s mostly about changing what our goals are. It’s focusing on helping people achieve the priorities that are most important in their lives. And that’s what I want when I’m older.
MJ: On a final note, have you given any serious thought to your own demise and how you want it to play out?
AG: [Laughs.] My wife and I have talked about this. For me, my cognitive function is fundamental to who I feel like I am. So if I became just a brain in a jar—as long as I can communicate back and forth with people, that would be okay with me. But if my brain goes, let me go. My wife, on the other hand, feels like, “Look, if I look happy, that’s gonna be good enough for me.” [Laughs.] I think the other lesson is that both of us may change our minds. Our ideas of what our priorities are shift as we come face-to-face with some of the struggles. So you have to have these conversations repeatedly. You have to be able to discuss what outcomes are really not acceptable to you. What are the fears and worries you have? Because they’re going to change as you gain experience.
MJ: And when you’re facing your mortality.
AG: Yeah. You may be more at peace. You may be incredibly more anxious about it. You may be in denial. Those are all totally normal things. Totally normal. And we should be capable of offering people clinicians who understand that and know how to help. It’s not that complicated.