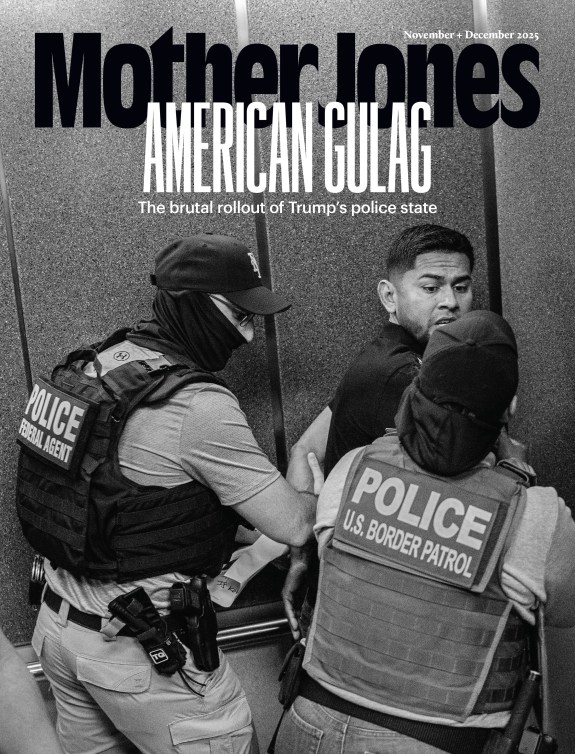
Sika Eteaki.Photograph by Annie Tritt
Sika Eteaki lay in bed, shaking uncontrollably. The pillow and sheets were soaked through with sweat, but now he couldn’t get warm. It felt like there weren’t enough blankets in all of Lancaster State Prison to keep him warm.
Just a few months earlier, Eteaki had turned himself in for illegal possession of a firearm. He’d been arrested with a gun while driving back from a camping trip. He and his family had used the pistol for target practice, for fun, but a spate of nonviolent priors from the decade before had prosecutors threatening to put Eteaki away for years. Since those early arrests, Eteaki had turned his life around. He now had four kids under five, a renewed faith in Mormonism, and steady work at a foundry. The prosecutor went easy, and after months of negotiation, Eteaki pleaded guilty to felony firearm possession and got eight months in Lancaster, on the outskirts of Los Angeles. In July 2010, Eteaki’s wife, Milah, drove him to the Long Beach courthouse, outside LA, where he surrendered and entered the system.
A hulking if slightly overweight presence, Eteaki stood 5-foot-10 and weighed 245 pounds, with broad shoulders, tattoos, and close-cropped black hair. His family was from the Polynesian archipelago of Tonga, and he’d arrived at Lancaster a strong, healthy man. But a few months into his stay, he started getting headaches and running a fever. He’d landed a plum job in the prison’s cafeteria and didn’t want to risk losing it by calling in sick, so he suffered through what he figured was a particularly rough flu for a week. He stopped by the prison clinic and was given ibuprofen and told to drink more water. He didn’t get better. He went back to the clinic and got more of the same. After a few more days of delirium, Eteaki learned from another inmate how to get the docs’ attention: “Tell them your chest hurts.” The next day, he was admitted to the prison’s hospital with a high fever and a diagnosis of pneumonia.
The prison hospital cell was cold concrete. Doctors set up intravenous drips and pumped him full of antibiotics. Eteaki asked what he was getting, but answers weren’t forthcoming; they were making him better, they said. But his fever wouldn’t recede. For days it hovered around 103, 104. He was drowsy and couldn’t eat. He also couldn’t write or receive letters in the medical wing, couldn’t tell his wife where he was or why he’d been ignoring the letters he knew she sent daily.
After three weeks of isolation in the clinic, he heard chains outside his door. Guards came in and ordered him to change into an orange jumpsuit. They shackled his wrists and ankles, strapped a surgical mask over his nose and mouth, and transported him to a hospital in Lancaster. There, chained to a bed, he continued to deteriorate. Doctors came and went, performed tests, and cycled him through a series of drugs. He lost more than 40 pounds. And still, no one seemed to know what was wrong with him.
One night, as Eteaki drifted in and out of consciousness, someone came in and asked for his emergency contacts. “Holy shit,” he thought, “they don’t know what to do with me. They’re just going to leave me here.” He tried to sleep, but the chills and hacking cough and fear were too much. He cried and thought of his wife and children. He remembered the hymns he’d learned in church as a child. “I need thee, oh, I need thee,” he sang.
For centuries, residents of California’s Central Valley have fallen ill with a mysterious disease that seemed to come with the great swirls of dust that periodically swept across the landscape. The illness, which killed some of its victims and left others debilitated and frail, appeared to choose its prey at random.
Valley fever, we know today, is born of a microscopic fungus that thrives in the valley’s fertile soil. Unlike most other infectious diseases, it does not spread through person-to-person transmission, but rather through dust particles that make their way into our lungs. Each individual fungus is a spore, a single-celled organism capable of asexual reproduction. When kicked up by cars or backhoes or tractors, spores can float across a county in an afternoon. They thrive in the dusty, dry swath of land that cuts from California to Texas, and billions of them are sent into the air with each subdivision we carve out from unclaimed expanses. Outside cities like Bakersfield or Fresno, you may inhale hundreds of these invisible fungal specks in a day. For most people, however, breathing in a few spores amounts to nothing—60 percent of people who inhale the fungi feel no symptoms at all. Thirty to 35 percent develop illness—usually flulike symptoms. Most people never even know they encountered the fungus—and for that reason, experts believe that valley fever may be much more common than official reports suggest.
But in 5 to 10 percent of the people who inhale the spores, the illness develops into something much more serious. The fungus is unrelenting. The airways in your lungs are laid out like an upside-down tree, and the spores do not rest until they reach the outer branches. There, past your lungs’ natural defenses, they settle at the terminus of your respiratory system, lodging themselves into the air sacs. The spores reproduce and grow fat with hundreds of mini-spores until they burst, releasing hundreds of new spores. Every bit of tissue touched by one of these new spores becomes inflamed as the fungus cascades across your respiratory system.
If you’re particularly unlucky, you get what’s known as disseminated valley fever: The fungus continues to spread out of your lungs and into your bloodstream. From there, it attacks any organ it can find, causing chronic pain, fever, and exhaustion. If you’re extremely unlucky, the fungus reaches your meninges—the membranes that envelop your brain and spinal cord. The lining of your brain begins to swell and the pain becomes unbearable as the pressure inside your cranium spikes. The infection cuts off the blood supply to your brain, depriving cells of oxygen. Finally, as the meninges grow more inflamed, your swollen brain has nowhere to expand but out of the base of your skull, a process called cranial herniation. And from there, death isn’t far off.
No one knows why some people develop life-threatening bouts of valley fever and others don’t. What is known is that for certain racial groups, the risk of contracting disseminated valley fever is much higher. For black men, it is as much as 14 times that of white men. Filipinos and Pacific Islanders like Eteaki are also thought to be highly susceptible, though there is not enough data to prove how much.
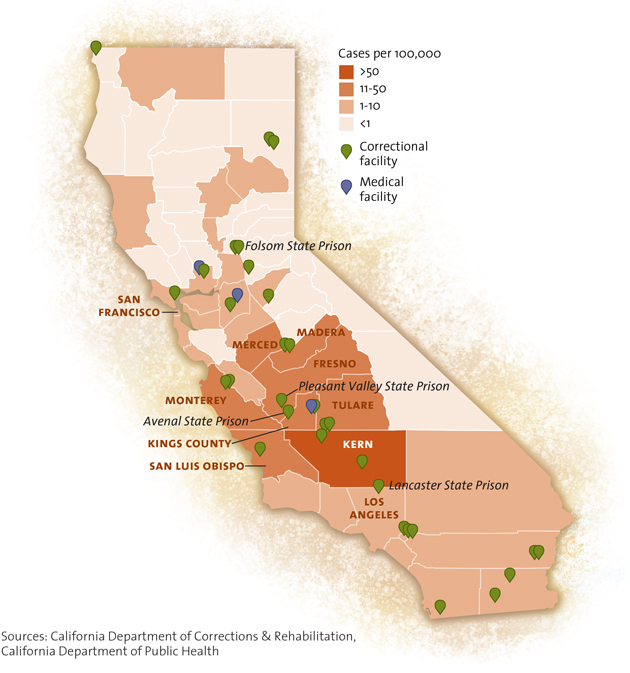
In California, the quirks of valley fever’s pathology have collided with the state’s habit of jailing a disproportionately large number of black and brown people. For years, the California Department of Corrections and Rehabilitation housed many of these minority inmates in prisons scattered throughout the dusty, endemic areas of the Central Valley. Thousands fell ill and dozens died. The story of their suffering is one of incompetence and outright negligence—it’s the story of how the state of California left thousands of its charges to suffer while under its care. If valley fever was endemic to the hills above Rodeo Drive or the boulevards of Palo Alto and struck down Caucasians with the ferocity it lays out African Americans, it would be the kind of public health emergency that sends Anderson Cooper into the field with a face mask. As it stands, valley fever remains, in the words of the Centers for Disease Control and Prevention, a “silent epidemic.”
Valley fever is technically called coccidioidomycosis and shortened to “cocci” by those in the know. It’s a poorly tracked disease, but to the best of anyone’s knowledge, around 20,000 Americans report coming down with it each year, and an average of 170 die. Those figures are likely an underestimate; the CDC has not released updated valley fever fatality statistics since 2008. But in an average year we can be sure that the disease kills more Americans than West Nile, hantavirus, rabies, and Ebola combined.
What’s more, the incidence of the disease has been rising—from 2,271 cases in 1998 to 22,641 in 2011. Whether the spike was because of new, more-thorough testing, a real rise in disease, or some combination of the two is unknown—and for equally poorly understood reasons, the number of cases has declined in the past few years. (There were 9,438 cases in 2013.) Nevertheless, it’s a trend that experts believe will continue to climb as the combination of drought, intensive agriculture, and climate change turns more of the American Southwest to dust. Bursts of rain followed by long dry spells—a pattern familiar to Californians—may be ideal growing conditions for cocci spores, and as climate change ensures that more soil stays arid and parched, the disease will travel with greater ease on gusty days in the Central Valley.
“Damn, what happened to you?” the inmate across from Eteaki’s cell asked. When Eteaki had left his cell in Lancaster, four weeks earlier, he’d weighed 245. Now he was down to 205, gaunt, his face sunken. After a week in the hospital, his fever had finally broken, and doctors told him he had valley fever. Almost immediately, he’d been dressed, cuffed, and hauled back to Lancaster. He began to read the pile of mail that had stacked up in his absence, watching as his wife’s correspondence grew more frantic with each unanswered letter.
That Sika Eteaki, a Tongan American from Long Beach, could end up with a little-known, often-misdiagnosed fungal disease in a Mojave Desert prison may seem like a quirk of circumstance and geography. But the seeds of Eteaki’s illness were planted three decades ago, when the California Department of Corrections decided that the Central Valley area was an ideal spot to park a ballooning prison population. The department built prisons in cities like Avenal, Corcoran, and Coalinga—dusty places that scientists would later learn contained some of the highest rates of valley fever in the state. Eight prisons were built in areas public health officials now consider “hyperendemic.” California was laying the groundwork for a public health catastrophe.
For most long-term Central Valley residents, the disease is a fact of life. Researchers speculate that many people there develop immunity, possibly by inhaling small amounts of cocci spores. Most locals who catch cocci suffer flulike symptoms (or nothing at all) and won’t get it again afterward. But California’s prison population is mostly made up of people from outside the valley—sitting ducks. And, especially in recent years, there have been a lot of them. The Central Valley is where 16 of the state’s 33 adult prisons are located. The inmate population for the state increased from roughly 25,000 in 1980 to 117,000 today. Before a federal order to reduce prison populations was handed down, the state had at least 40,000 more inmates than it had prison beds. The inmates lived like factory-farm cattle. Thousands slept in triple-decker bunk beds erected wherever space could be found. Tough-on-crime ordinances—particularly the “three strikes” law—also led to a huge influx of minority inmates. Today, African Americans make up just 6.6 percent of California’s population, yet they represent a full 29 percent of its prison population.

Beginning in 2005, cocci began tearing through the populations of several Central Valley prisons. The rate of infection inside a few of these prisons was at that time dozens of times higher than in neighboring towns. At one, where a large construction project had just been completed next door, inmates were 400 times more likely to contract cocci than the people living nearby. When Eteaki entered the system four years ago, he landed in a veritable hothouse for valley fever.
Since 2005, around 4,000 California inmates have developed valley fever, and 53 have died from it. For survivors, the infection does not go quietly; devastating symptoms can persist for years after an inmate leaves prison. What’s more, fungal infections are famously hard to treat; unlike bacteria, fungal cells closely resemble human cells, meaning it’s difficult to find drugs that will zap the fungus and leave the human ones intact. Anti-fungals are toxic to both the fungus and the host, often causing headaches, nausea, dizziness, and rashes in patients, along with less frequent but more frightening side effects like seizures and liver failure.
Valley fever, if not a death sentence, can still become a life sentence—a burden that will follow former inmates to their grave—and one that the state refuses to help pay for.
Doctors diagnosed California’s first recorded case of valley fever in 1893, in a Central Valley field-worker from the Azores islands. An eminent pathologist from Johns Hopkins University theorized, incorrectly, that the attacking organism was a parasite similar to one commonly found in dogs, coccidia. The researchers named their mysterious organism Coccidioides (“resembling coccidia”) immitis (“not mild”). The disease went on to baffle doctors for decades. During the Second World War, the Army built airstrips into the dry earth near Bakersfield, releasing spore-laden dust and sickening hundreds of US airmen. German POWs and interned Japanese Americans being held in Arizona also came down with valley fever at staggering rates. The Germans were relocated. The Japanese Americans, according to oral historian and medical anthropologist Gwenn Jensen, were not.
After the war, infection became more common among oilmen, construction workers, and others who spent their lives rooting around in the dust. In 1972, 17 out of 39 archaeology students developed the disease while excavating an ancient Native American site in Red Bluff, California, then thought to be miles north of the endemic zone. Later, centuries-old human remains discovered at the site were found to show evidence of valley fever.
And yet, despite its long history, valley fever is still not very well understood. Medical professionals in the affected areas call valley fever an “orphan disease.” Rarely does the ailment attract attention outside of the hardest-hit parts of California and Arizona—and research dollars are hard to come by. Though some progress has been made on a vaccine, researchers say the millions of dollars needed to finish it aren’t coming anytime soon. “It’s always viewed as a highly regional specialty, so it’s always struggled to get a broad research base,” says Michael Lancaster, the former head of the Kern County Public Health Laboratory, one of the few labs in the country equipped to confirm a valley fever diagnosis. “It’s a little bit frustrating. West Nile virus swept across the country. People died from West Nile—there’s no question. But if you look at the overall impact, it was nowhere near cocci. And [West Nile] got so much funding.”
Outside academia, county health officials in the endemic zone are the closest thing to experts that valley fever has. Dr. Mike MacLean, the public health officer of Kings County, an underpopulated area in the middle of California, has witnessed one of the worst cocci outbreaks in the state. His county has only 150,000 or so residents, but it’s also home to Avenal State Prison, a perennially overcrowded medium-security institution that, along with nearby Pleasant Valley State Prison, was ground zero for the cocci outbreak that began in 2005. With tanned cheeks and a thick white mustache, MacLean looks like he might rustle cattle on his days off. But he speaks with urgency and an unexpected passion. He is measured, but doesn’t suffer bullshit or mince words. “I’m sure none of this would have happened if they weren’t prisoners,” he told me.
To understand the prison system’s botched response to the festering outbreak, you need a quick history lesson. On April 5, 2001, the Prison Law Office, a nonprofit law firm in Berkeley, filed the largest class action suit in the state’s history against the California Department of Corrections. In it, attorneys alleged that the system was providing prisoners with medical treatment so poor as to be unconstitutional. Among the most shocking charges was that, on average, an inmate died every week due to inadequate care or malpractice. The state, likely because it was aware that conditions in the prisons quite possibly qualified as cruel and unusual punishment under the Constitution, acquiesced and agreed to implement “comprehensive new medical care policies and procedures at all institutions.”
Over the next few years, the state Department of Corrections claimed that it was cleaning up its act, even adding “rehabilitation” to its name. But three years after the settlement, court-appointed experts found that between 20 and 50 percent of physicians employed by the California Department of Corrections and Rehabilitation (CDCR) provided poor care; that many of the doctors had criminal pasts or revoked hospital privileges; that inmates were consistently misdiagnosed and ignored; and that 80 percent of high-level management positions in the health care services division were vacant. As former California undersecretary of corrections Kevin Carruth put it in testimony, “It never will be the business of the Department of Corrections to provide medical care.”
In 2005, Judge Thelton Henderson ruled that the CDCR had not kept its part of the bargain. The prison health care system, he wrote, was “broken beyond repair.” With a single order, he stripped the department of its power to control the prisons’ health care system and placed a federal official in charge. The official, known as the receiver, was tasked with fixing the “unconscionable” mess the prison system had created. If the corrections department was ever going to get out from under this federal receivership, dozens of new medical facilities would have to be built, thousands of hospital beds would have to be added, and the prison system would have to prove that it could and would provide inmates with adequate care.
But even as Henderson and prison officials were hashing out an arrangement in San Francisco’s federal courthouse, the cocci outbreak was beginning to take hold 160 miles south. By the fall of 2005, 166 prisoners at Pleasant Valley State Prison had come down with valley fever. It was a galling number, even for a patch of Fresno County more than familiar with cocci. In Pleasant Valley’s 20-year history, valley fever had been a regular concern, but this year was different. The rate of infection had tripled, and almost a fifth of the stricken needed hospitalization—an unusually high percentage. Four inmates had died. At Avenal—15 miles south, in Mike MacLean’s county—47 inmates had contracted the disease so far.
A team of state epidemiologists arrived at Pleasant Valley to investigate the spike in cases. Dr. Janet Mohle-Boetani and Dr. Charlotte Wheeler went through the obvious options first. Had the prison started testing more frequently? Or hired new doctors? Or sent out for more lab results? No, no, and no. Cocci infections are dictated by environmental conditions—the spores multiply after rainy seasons, then cause an uptick in cases once the soil dries and the cocci-filled dust begins to swirl. Maybe it had been a big “grow and blow” year and numbers were up everywhere? No, infection rates within the prison were drastically higher than in the surrounding community and the state as a whole. To top things off, next door, about 500 feet from the walls of Pleasant Valley State Prison, the state had spent months clearing a large patch of land and constructing a sprawling, multistory mental-health facility.
In late 2013, I drove to the suburban Sacramento office complex that the federal receivership calls home. Mohle-Boetani now works for the receiver and is technically the deputy medical executive for the public health unit of California Correctional Health Care Services. A Berkeley- and Stanford-trained physician and epidemiologist, she strikes a very doctorly figure: lightly graying hair, studious glasses, and the air of someone who doesn’t doubt what she’s saying. She first crossed paths with cocci more than a decade ago, when she was working as an officer for the California Department of Public Health, investigating a potential tuberculosis outbreak in the eastern San Joaquin Valley. Many of those cases, she realizes now, were likely valley fever.
Valley fever is in a completely different class from your typical prison disease outbreak, she told me. Prisons are and always have been breeding grounds for infectious diseases, she said, and as a result there are some standard responses—typically to isolate and quarantine. But you can’t quarantine people from the very air they breathe. “I think it’s one of the most difficult problems to deal with in public health,” Mohle-Boetani said. She motioned to a photo she keeps tacked to the wall of her office, an aerial shot of Pleasant Valley State Prison, surrounded on all sides by dusty open fields. “How do you separate people from their environment?”
At first, says Wheeler, she thought the disease might contain itself. She reasoned that the inmates who recovered from valley fever would gain immunity and the outbreak would die out. But the prison system’s habit of regularly transferring inmates between institutions ensured that there would always be fresh victims in Pleasant Valley.
In January 2007, Mohle-Boetani and Wheeler recommended a two-pronged strategy. The first was a series of environmental changes to reduce inmate exposure to dust: shrubbery planted in the open fields nearby and limited time outdoors. Second, the team said that the inmates most at risk should be removed from the environment. They recommended transferring out African Americans, Filipinos, and individuals with compromised immune systems.
In late 2010, Eteaki was transferred to the California Rehabilitation Center in Norco, 50 miles east of LA. After he told a doctor about his condition, Eteaki spied the physician Googling “valley fever.” Norco sits adjacent to a palm-lined artificial lake in an area not known for the disease. The prison itself occupies a grand, eight-story Spanish-style manor—the remnants of the Norconian Resort Supreme, a famed hotel that once attracted Hollywood stars. Purchased by the Navy during World War II, it was given to the state in the 1960s.
At Norco, Eteaki’s valley fever came raging back. Breathing became difficult, and he was overcome with exhaustion. He developed a bulging, globular growth on his neck. He lost another 25 pounds, for a total of 65. The prison’s layout didn’t help matters. Eteaki was being held on the third floor; the clinic was on the eighth. There was no elevator for inmates, and each day he wheezed up and down the five flights of stairs for his meds. He worried about passing out from the exhaustion. On each floor, guards implored him to speed up. “What the fuck are you doing? Hurry the fuck up,” one guard told him. “Don’t come to jail if you can’t breathe.” In the clinic, a doctor told him that his cocci had disseminated, escaping his lungs. The doctor was worried that the disease would find its way to Eteaki’s brain and lead to fungal meningitis. You could die at any time from this, he warned, and he prescribed Eteaki an inhaler for the breathing difficulties.
A few weeks later, with three months left in his eight-month sentence, Eteaki’s vitals declined. Once again he was cuffed, masked, and driven to the local hospital. There he was placed in the biohazard room, even though valley fever isn’t passed from person to person. He felt like the monkey in the movie Contagion. His “titer count,” the metric doctors use to estimate the concentration of fungi in the body, was dangerously high. That night, he was given an intravenous drip to push back the fungus. The neon-yellow liquid caused a negative reaction as soon as it entered Eteaki’s bloodstream. He felt like he was being stabbed from the inside. Handcuffed, he struggled in vain to hit the panic button and halt the flow, finally throwing himself on the floor and tearing off his tubes and monitors in the process. The nurse who responded chided him for making a mess. A few days later, his titer count dropped and he was sent back to Norco. This is the pattern of valley fever: bouts of relative calm followed by relapses of the life-threatening, spirit-sapping illness.
When Eteaki got back to Norco, his wife planned a visit. He hadn’t seen his children in months, and he asked Milah to bring along their oldest son, then four years old. Eteaki and the other inmates were searched and led single-file into the visiting room. When Eteaki shuffled through the door, his wife looked right past him. He was 65 pounds lighter, and his head had just been shaved to check for signs of meningitis. He looked hollowed out. When Milah finally recognized the spindly man as her husband, she burst into tears. Looking down at his son, Eteaki saw fear in the boy’s eyes.
At Pleasant Valley State Prison, the 166 reported cases of cocci in 2005 had swelled to 514 by 2006. In the year since Mohle-Boetani and Wheeler had visited, the outbreak had exploded, exceeding the worst expectations. At Avenal State Prison, 91 cases were reported. An esteemed valley fever expert at the University of California-Davis calculated that almost a third of cocci cases in the state originated in the prisons—up from 15 percent a year earlier.
When the corrections department received the epidemiologists’ draft report, late in 2006, it acted with relative speed, agreeing to remove immunocompromised inmates from the affected prisons. However, despite Mohle-Boetani’s recommendation to remove African American and Filipino inmates—nearly all of the cocci literature dating back to the 1930s notes the increased risk to these groups—the department decided to keep those inmates exactly where they were. (The California Department of Public Health can make recommendations, and the CDCR can elect not to carry them out.)
Most of Mohle-Boetani’s other suggestions were ignored too. One of the key recommendations was to pave the ground around the prisons, a technique that had proved successful during World War II, when it had been used at Central Valley military bases, cutting cocci infections by between one-half and two-thirds. Covering the dusty expanse around the prison with concrete could reduce the number of cocci spores in the air, experts reasoned. But in January 2007, Pleasant Valley’s warden, James Yates, balked. The initial cost was estimated at upward of $750,000. In the end, the department opted for a cheaper alternative: chemical sprays and gravel cover to stabilize the soil. At the time, medical care for inmates with valley fever was costing the state $23 million a year.
In 2007, a few months after the epidemiologists had issued their recommendations on valley fever—and the CDCR had ignored them—the department asked a separate delegation of county health officials to meet and discuss how the disease could be curtailed. The group, which included Kings County’s Mike MacLean, made 26 detailed recommendations, from simple landscaping to funding vaccine research. “If no significant improvement is made,” the last recommendation reads, “consider relocating all inmates.” Of the 26 recommendations, the CDCR pursued a total of 4.
Eteaki spent his last two weeks as a prisoner in the Norco clinic. Doctors were concerned that he was too sick to be released, but he begged. On March 30th, 2011, his wife picked him up and drove him back home to Long Beach.
When sick inmates are released from California’s prison system, they’re given a 30-day supply of medicine, regardless of their disease. Eteaki was jobless and uninsured. His condition worsened after his prison-issued anti-fungal drug—called Diflucan—ran out, and he began going to the emergency room for treatment. For Eteaki and the thousands of other prisoners who contracted valley fever behind bars, the cost of treatment came as a shock. A 30-day course of Diflucan was about $550, but prison doctors had Eteaki on a double dosage because of the severity of his disease, so his treatment was twice as expensive. He asked the prison system for help, but it refused. He and his wife sought aid through Social Security and Medi-Cal, but they were told there was nothing anyone could do—because Sika’s wife was working full time and the couple had savings, they did not qualify for assistance. He began to take fewer pills to try to stretch the bottles out. Between the hospital visits and the pills, Eteaki spent more than $20,000 managing the disease, burning through all his savings—money he had hoped would help support his wife and children.
Eteaki’s family helped him pay bills, but he felt ashamed for asking. One day, a few months after he was released, he lay on his mother’s couch, sweating, moaning in pain. His mother began to call an ambulance, but he begged her not to; he couldn’t afford the cost. Eteaki’s mother and father had come from Tonga and lived the American Dream. His father made good money working at the foundry where Eteaki had been employed, and the family had never wanted. “We came out here for you guys to have a better future,” his mother said as they drove to the hospital.
In one short year, valley fever had become the scourge of the Eteaki family. While Eteaki was in Norco, his younger cousin Mosese fell ill after taking a construction job in Arizona. When he returned to Utah, where he lived with his family, doctors were unable to diagnose him. He flew to California for tests, learned he had disseminated valley fever, and died five months later. He was 18 years old.
In 2012, the federal receiver recommended that the CDCR immediately transfer anyone categorized as “high risk,” including African American and Filipino inmates. The court’s experts agreed, as did the state’s public health department and its epidemiologist, but the corrections department didn’t do it.
In June 2013, the department’s attorneys wrote a legal brief outlining why it should not be forced to hastily remove a large portion of the population from the affected prisons. Instead, they argued, officials should wait for “experts from the Centers for Disease Control and the National Institute for Occupational Safety and Health [NIOSH] to complete their study and evaluation before implementing such a drastic remedy.”
But the experts at NIOSH had been called in before—four and a half years earlier. In late 2008, officials from the prisons’ Office of Risk Management, which oversaw occupational health and safety and workers’ compensation, had sent a formal request to the agency, asking the epidemiological experts there to visit Pleasant Valley and Avenal to help the prisons reduce guards’ and workers’ risk of catching cocci. At least two workers had already died of the disease. NIOSH agreed to send two epidemiologists out to California for a site study. But at the last minute, the investigation was called off. At the time, no reason was given.
Prison officials are tight-lipped about why the federal government’s epidemic experts never investigated the cocci outbreak, but emails and public records obtained from the counties, prisons, and CDC through Public Records Act and Freedom of Information Act requests show that despite a concentrated effort from a few public health employees inside the corrections department, prison officials killed the NIOSH health evaluation request.
One of the reasons, it seems, had to do with a mandate from the receiver to increase the number of medical facilities across the system and add thousands of beds to alleviate overcrowding. The state Legislature had just ponied up $7 billion for the task. In emails, members of the construction team wondered what effect building new facilities would have on the inmates and surrounding cities in the endemic zone: Would more people get sick if they disturbed the soil during construction and let more cocci spores loose? The fear of potential outbreaks could force the department to halt construction on the buildings they needed to meet the receiver’s requirements and end the federal receivership. After department officials made the initial investigation request to NIOSH, prison employees appeared worried. “What will happen if [the review] leads to recommendations that we do not think are feasible?” one asked NIOSH’s lead investigator as the evaluation date neared. “Does the media typically become aware of [NIOSH’s evaluations]?”
Seven days before NIOSH’s scheduled visit, the CDCR Office of Risk Management’s lead health official, Dr. Nikki Baumrind, sent an email to Dr. Marie de Perio, NIOSH’s point woman on the case. “Could you pls give me a call at your earliest convenience?” she wrote. That night, emails show, Baumrind called de Perio to say that the study would have to be delayed. Instead, an advisory panel was to be convened to address whether a NIOSH investigation was even necessary.
In notes from a later conference call, Baumrind is quoted as saying that the trip was postponed because of concern about the department’s obligation to respond to NIOSH’s recommendations.
For a few weeks, de Perio and state officials, including Baumrind, frantically searched for a new “sponsor” to call NIOSH in. The heads of the prison-guard unions—representatives of the very people the workplace-safety study was intended to protect—declined or ignored the request. California’s independent public health department felt it was not appropriate to take the helm “in light of concerns that without full engagement from CDCR, the request would not lead to a successful outcome.”
Then, in June 2009, the corrections department shuttered its own Office of Risk Management. In the four years after the CDCR canceled the workplace health and safety study, three correctional officers died of valley fever.
“We had the opportunity to have a quality study performed at no cost to California,” MacLean wrote in an email to the director of the California Department of Public Health a few weeks later. “Cocci morbidity and mortality will continue regardless of our choice to ignore it. I think it’s a sad comment on the state of public health in California.”
In July 2013, lawyers representing several inmates at Pleasant Valley State Prison filed a class action lawsuit against the state. The suit alleged, among other accusations, that the CDCR and the state failed to protect and care for inmates vulnerable to cocci at several Central Valley prisons. The treatment that incarcerated valley fever patients received—and the system’s unwillingness, for seven long years, to exclude at-risk inmates from the endemic prisons—constituted negligence, and was tantamount to cruel and unusual punishment, violating the Eighth Amendment. This wasn’t the first time a prisoner had sued over valley fever. In 2009, a former inmate of the federal penitentiary in Taft, a small town at the southern end of the Central Valley, sued the federal government for “recklessly” exposing him to cocci. The feds settled and agreed to pay him $425,000.
The 2013 lawsuit listed case after case of prisoners with valley fever receiving subpar care. According to state reviews of inmate deaths, in 2008 a 26-year-old inmate told a prison nurse that he’d lost 10 pounds in the past month and suffered from chest pain and a constant cough. He was referred to a physician, but no appointment was made for him. Two weeks later, he submitted a request for care, writing, “Emergency. I would like to see the doctor ASAP.” There is no record of a response from the clinic. Ten days later, he was 20 pounds lighter. After he was finally sent to a local hospital, doctors confirmed he had advanced cocci, but the infection had progressed too far to treat. The man died of renal and respiratory failure 10 days later.

In 2009, prison health care providers failed to evaluate two prisoners; one had lost 56 pounds and suffered from consistent fever, cough, and chest pain. One had not been prescribed anti-fungal medication for two months. They both died soon after.
In 2010, when a 68-year-old inmate had a recurrent case of valley fever, doctors didn’t consult with a specialist until the man was near death. At a local hospital, a unilateral “do not resuscitate/do not intubate” order was written by physicians. There are no records showing that the inmate, who died a few days later, was consulted.
In 2011, specialists failed to recognize that a 42-year-old HIV-infected man diagnosed with pneumonia had in fact been suffering from disseminated valley fever. He died.
In 2012, a 45-year-old black man told prison doctors he’d lost 20 pounds in the past six months. The attending physician checked a box on his medical chart indicating the man was at high risk for valley fever, but no testing was done for the disease. Three months later, after precipitous weight loss, the man entered the clinic in an altered mental state—a clear sign of meningitis—and was finally diagnosed with cocci. He died the next month.
Dr. John Galgiani, a professor at the University of Arizona and one of the world’s leading experts on valley fever, later wrote in a review that the prison medical system’s response to the cocci outbreak was unacceptable, noting that the medical staff in the middle of the endemic zone was slow to recognize the signs of valley fever, particularly in African Americans, even years after the outbreak began. “As a result,” wrote Galgiani, “needless suffering and death were inflicted on these men.”
Arthur Jackson, a black inmate at Pleasant Valley, caught valley fever in 2011. “Two years after contracting this disease, I suffer from loss of vision, severe and often debilitating headaches and joint pain, weight loss, fatigue, and numerous other ailments for which I am consistently denied treatment,” he wrote to me. “I often wonder if this disease were to have affected all races alike, would the response of prison officials have been the same or would more have been done to protect and treat us?”
“Living with valley fever in prison is simple,” Pleasant Valley inmate LaCedric Johnson wrote to me. “You live every day like the last till you die.” Johnson, who was convicted of carjacking and assault, contracted the disease in 2011. He’s experienced lung damage, fever, chills, sweats, headaches, aching joints, severe weight swings, fatigue, sleeplessness, and loss of concentration. Like Eteaki, he was prescribed Diflucan. “Who gives a fuck,” he wrote, “if a few thousand inmates are housed in a prison built on soil that contains a fungus in the ground that kills African Americans at a high rate?”
As the inmates’ case winds its way through federal court, much of it will likely revolve around whether officials should have removed inmates from prisons in the hyperendemic area sooner. A key goal, attorneys say, is to force the state to cover the health care costs of former inmates who contracted valley fever in prison. One study found that many long-term valley fever patients, like Eteaki, spend tens of thousands of dollars on care, on top of the cost of hospital visits.
And while the prison system argues that it didn’t know how bad the problem was—or didn’t have the capacity to handle it—the attorneys say that doesn’t wash. Nazareth Haysbert, one of the lawyers involved, told me, “It’s a special irony that the US and California would knowingly confine US citizens, albeit prisoners, to the same areas—known to cause deadly outbreaks of cocci—from which they had removed Nazi prisoners of war mere decades earlier.”
In October 2013, I called Eteaki and asked how he was doing. Things had been looking up for a while—with regular doses of Diflucan, he gained back some weight, went to work full time, and even began taking some community college classes. But when he stopped taking his Diflucan because he couldn’t afford it, the disease invaded his right index finger. His doctor recommended amputation to stop the fungus from spreading; a side benefit would be that he’d quality for disability, which would pay for the Diflucan. Eteaki was despondent. “I’m doing welding,” he said. “How can I work without my finger?”
That November, I visited Pleasant Valley myself. By that time, all the African American and Filipino inmates were gone—more than a year after the receiver urged CDCR to transfer prisoners whose racial or ethnic backgrounds put them at high risk for valley fever, the department finally complied. Officials took me on a show-and-tell tour. I saw what court-mandated steps had been taken to help halt the spread of the cocci spores. I saw new ventilators, door seals, and informational signs about the dangers of dust inhalation. I was told CDCR would start screening all inmates for valley fever with a new skin test, in January 2015.

Eteaki had told me about his cousin Johnny Kalekale, who’d robbed a liquor store at gunpoint a few years earlier and was now serving a multiyear sentence. It was Johnny’s younger brother, Mosese, who’d died of valley fever that he contracted at an Arizona construction site. Eteaki told me that Johnny had just been transferred to Pleasant Valley, sent to fill one of the vacancies left by the black and Filipino inmates—Pacific Islanders were not included in the transfer order. Johnny says he had told the transfer committee that his brother had died from valley fever, but this had changed nothing. (CDCR maintains he did not advise it of his brother’s death.)
I wanted to meet Johnny, but I wasn’t allowed to interview specific inmates. I was, however, allowed to wander the yard and talk to random prisoners. I met an older man, Nicolas Moran, who said that he’d had valley fever for several years but the doctors were refusing to treat his latest outbreak. He was in pain, he said. He begged me to tell his story. “We’re human beings too,” he said. “What’s the difference between us?”
I sent Johnny Kalekale a letter. In his reply from Pleasant Valley, he wrote, “I honestly felt like they were sending me to my death. I won’t let my wife bring my kids, for fears they might catch it. I know I’ve done things to end up here, but I hope I don’t leave this world because of VF.”