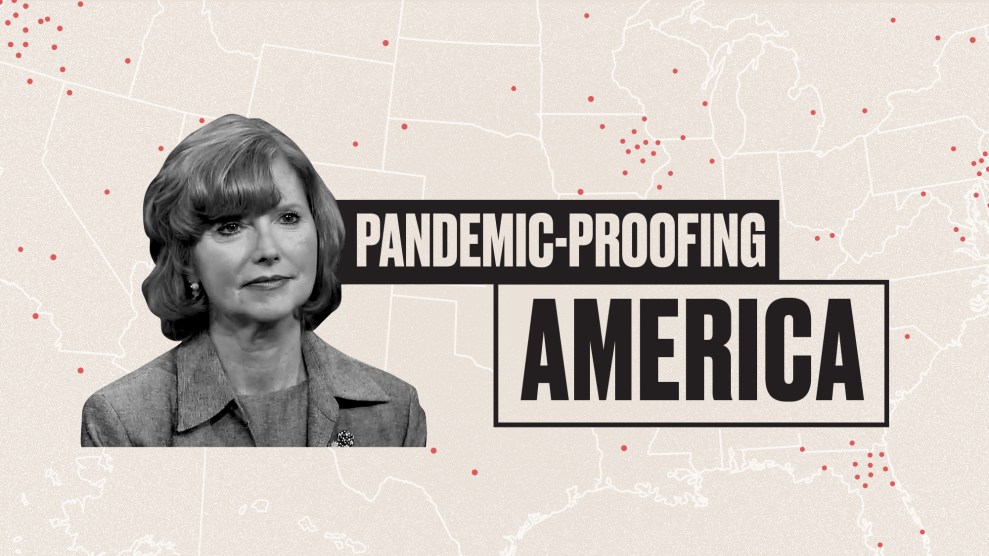
Mother Jones illustration; Matter of Fact with Soledad O'Brien
As the world grapples with the devastation of the coronavirus, one thing is clear: The United States simply wasn’t prepared. Despite repeated warnings from infectious disease experts over the years, we lacked essential beds, equipment, and medication; public health advice was confusing; and our leadership offered no clear direction while sidelining credible health professionals and institutions. Infectious disease experts agree that it’s only a matter of time before the next pandemic hits, and that one could be even more deadly. So how do we fix what COVID-19 has shown was broken? In this Mother Jones series, we’re asking experts from a wide range of disciplines one question: What are the most important steps we can take to make sure we’re better prepared next time around?
As the head lobbyist for the National Rural Healthcare Association, Maggie Elehwany is on the front lines of the battle over funding for rural hospitals that are struggling to survive. According to the Cecil G. Sheps Center for Health Services Research at the University of North Carolina, Chapel Hill, at least 128 rural hospitals have closed since 2010. Rural hospitals have long struggled because they serve smaller populations in areas that generally have high poverty rates. But in recent years, those challenges have been compounded by the decision made by many states with large rural populations to not expand Medicaid, making it harder for those hospitals to be reimbursed at reasonable rates. The COVID-19 pandemic only puts in starker relief what those hospital closures have cost the communities they serve, and it has meant more pressure on regional hospitals that are still standing. In April, through the CARES Act passed by Congress the month prior, the Department of Health and Human Services allocated $11 billion to rural hospitals. I caught up with Elehwany to learn more about how the coronavirus is exacerbating the health care crisis in rural America.
On the challenges facing rural populations: Even before COVID, we had a fragile rural health care safety net. In rural areas, it’s all about access to primary care, but if you need a specialist, that’s especially difficult. We have systemic workforce shortages—20 percent of the population lives in rural areas, but only nine percent of physicians practice there. Recruitment and retention have always been one of the biggest challenges in rural healthcare. The shortages are significant in other types of care too; think mental health and oral health. And rural populations are needy, they’re older, they’re poorer, they’re sicker, they have higher percentages of chronic disease. Rural areas have been dealing with the opioid epidemic, often they have riskier lifestyles and occupations, and higher percentages of smoking and drinking. All of those factors made them more vulnerable to the virus.
Complicating matters further is the hospital closure crisis in rural America. We saw a record number of closures last year, and this year, we were on track to see even more. So hospitals in cities are not only serving the populations within the city limits, but they’re also responsible for people in the surrounding counties, where hospitals may have shut down. By the time COVID hit, we already had half of all rural hospitals in the country operating at a financial loss. Then in preparation for the pandemic, hospitals were told to eliminate all non-emergency and elective care, which means decimating essentially 70 percent of those hospitals’ revenue. That was devastating.
On what rural communities need to fight COVID-19: We are asking Congress to help rural America be prepared as the pandemic swells. You may have 1000 cases reported in a community, but in the entire county, there’s just one hospital, and it’s a 25-bed critical access hospital. First and foremost, we’ve got to keep those hospitals—and all providers’ doors—open. The lifeline that was the CARES Act literally kept the doors open. It was a tourniquet, maybe it will save the leg, but if you take that tourniquet away, the patient is going to die. We’re asking for sustainable relief. We want to stop the cuts that are causing the closure crisis, but it’s also time to start thinking about new payment models for rural areas.
On how some providers are coping: Restrictions have been eased in telemedicine, including several requirements we’ve wanted to see loosened for a long time. We’re worried they’re going to flip the switch and say, OK, we’re going to end that now, the emergency is over. There’s a sense of isolation in a lot of senior populations and populations struggling with mental illness, and using telehealth can make such a difference. It doesn’t solve all of the problems, but it is cost-effective and helps people access care.
On the future of the coronavirus in rural America: We’re seeing the virus grow rapidly in rural areas where the meatpacking industry has set up shop, and in some prison populations; we’re worried that a lot of field workers and food processing plant workers are going to get sick. We’re worried that if people let their guard down, it’s going to be devastating in rural areas because of the vulnerability of the population.
Even with the influx of cash that the CARES Act provided, we still lost four rural hospitals since the pandemic began. We’re so worried that when the influx of relief stops, we’ll actually be in a worse off situation. Once COVID hits these communities, the hospitals will have fewer resources to fight it because of the massive loss of revenue. There are some estimates that those hospitals will never reach the levels they were operating at before, and even the “before” isn’t great because at least half of rural hospitals were operating at a loss.